What you’ll learn:
- People stop taking a semaglutide medication like Ozempic®, Wegovy®, or Rybelsus® for a variety of reasons.
- Regaining weight is a possibility for people who don’t have a firm plan in place after stopping the medication.
- Tapering off and building strong daily habits make maintaining weight easier once you stop semaglutide.
People stop taking a semaglutide medication, like Ozempic® or Wegovy®, for various reasons. Some are navigating cost or insurance changes, while others are dealing with side effects. Some have reached their goal weight, are considering a different medication, or are planning a pregnancy. Whatever your reason, stepping off treatment means your appetite and digestion will gradually shift back toward your personal baseline—and having a plan makes the transition smoother.
How you move forward often depends on how long you’ve been using semaglutide and why you were prescribed it. The approach can look different for people taking it for weight loss versus diabetes or heart health. Many people stay on the medication for 6 to 12 months, while others use it longer, taper off, or transition to another option based on what feels sustainable.
There’s no one “right” path here. Decisions usually come down to your health needs, side effects, cost, and what feels manageable over time.
If you’re preparing to stop semaglutide—or even just thinking about it—you’re probably looking for clarity on what happens next and how to maintain the progress you’ve made. Here’s what the transition typically looks like and the strategies that can help you stay on track.
What is semaglutide?
First, a little recap: Semaglutide is a GLP-1 medication that mimics a natural gut hormone called glucagon-like peptide-1 (GLP-1 for short). It’s the active ingredient in Ozempic®, Wegovy®, and Rybelsus®. Regardless of which version you’ve taken, they all work through the same GLP-1 pathway.
Semaglutide activates GLP-1 receptors throughout your body, lowering appetite, slowing digestion, and regulating blood sugar.
These combined effects help manage diabetes or help people lose weight. With the highest dose (2.4 mg), people have been shown to lose an average of 15% of their body weight in about 2 years.
Learn more: What is semaglutide? Exploring the weight loss benefits, side effects, and cost
Why people regain weight after stopping semaglutide
Once semaglutide starts leaving your system, the medication’s boosted GLP-1 activity fades, and your appetite control shifts back to relying on your body’s natural signals. That’s why weight regain can happen after stopping—especially without preparation or supportive habits already in place.
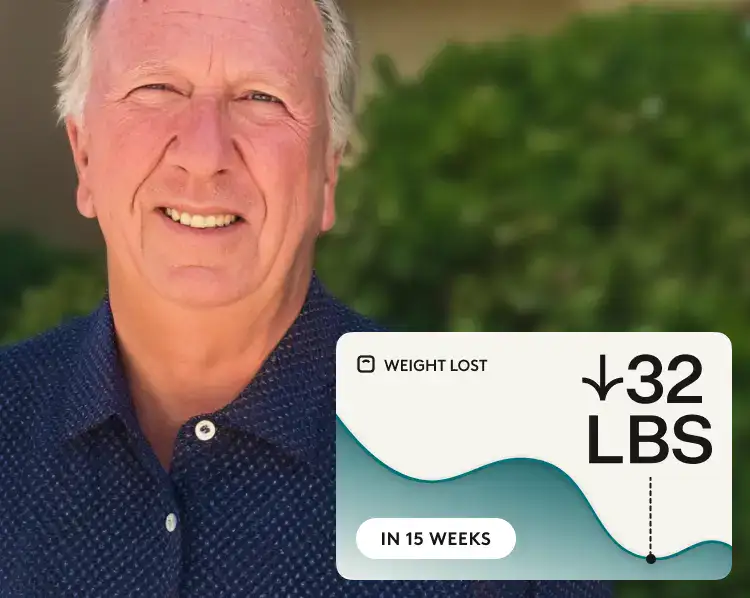
Research shows this pattern is common. One study found that people regained about two-thirds of the weight they lost within a year of stopping semaglutide. But with the right lifestyle support, that regain can be slowed. In another study, people who paired semaglutide with a structured lifestyle program lost slightly more during treatment and regained less afterward. A year after stopping, they were still down about 6% from their starting weight, compared with about 3% in those who didn’t receive additional support.
Learn more: What happens when you stop taking Ozempic® or Wegovy®?
How to reduce weight regain after stopping semaglutide
There’s no way to know exactly how your body will respond once you stop taking semaglutide, but research does offer some helpful guidance. Here’s what current studies highlight:
- Tapering helps. Data shows that personalizing doses and slowly tapering semaglutide while following a digital behavior-change program helped many people maintain their target weight for up to six months.
- Exercise matters. In one study, people who combined a GLP-1 medication with a supervised exercise program regained significantly less weight after stopping compared to those using medication alone.
- Healthy routines create stability. Regular movement, balanced meals, and structured habits provide the cues your body loses when semaglutide is no longer active. According to a study, people who added a lifestyle program alongside semaglutide kept more of their progress after stopping, underscoring why healthy habits make such a big difference.
So yes, weight regain is common, but understanding these patterns gives you more room to prepare and stay in control of your next steps.
Reasons for stopping semaglutide and what that means for controlling weight after
There isn’t just one reason someone steps off semaglutide—cost, hitting a goal, and side effects all play a part. You might also be weighing it against other weight loss medications like tirzepatide or thinking about switching. Knowing what prompted the change helps you figure out how to keep your weight managed after.
If you’re stopping because of cost concerns:
GLP-1 medications are often a long-term commitment, not a quick fix. Many people stay on them for at least a year, and some research shows people continuing treatment for up to four years. That’s a big time window, and it’s one reason the costs can add up, especially if you’re paying out of pocket. Typical list prices for semaglutide medication brands are:
These prices can make long-term treatment difficult to maintain, especially when insurance coverage is limited or unpredictable for weight loss treatments.
The next step: Look for ways to save, including manufacturer programs. Both Wegovy® and Ozempic® have a limited-time $199-per-month intro price for the first two months at the lower doses. After that, self-pay pricing through the NovoCare Pharmacy drops to $349 per month for most dose levels. The exception is the maximum dose for Ozempic® (2 mg), which stays at $499 per month.
Learn more about semaglutide costs:
- Ozempic® costs: With and without insurance
- Wegovy® cost: With and without insurance
- Rybelsus® costs: With and without insurance
If you’re stopping because of side effects:
Everyone reacts to semaglutide differently, and side effects are common when you first start the medication or your dose is increased. But some people find adjusting to the nausea, vomiting, constipation, or stomach pain difficult.
The next step: Talk to your provider about a dose change, slower titration, or even switching to another medication. Tirzepatide (Zepbound® & Mounjaro®) has been found to cause a bit less vomiting, constipation, and acid reflux than semaglutide for some people. If those are the side effects getting in your way, your clinician can help you decide if making a switch makes sense.
Learn more: Semaglutide side effects: Symptom guide & management tips
If you’re stopping because you’ve reached your goal weight:
Once you get to your goal weight, you may feel ready to try maintaining on your own.
The next step: Your provider can also guide you through a tapering plan to help maintain your progress. They also might suggest staying on a lower maintenance dose indefinitely.
Learn more: How to stop taking Ozempic® safely
If you’re stopping because weight loss has plateaued:
Plateaus are a common part of any weight-loss journey, and semaglutide is no exception. In one major trial, weight loss on semaglutide leveled off around week 60, then stayed fairly stable after that. This happens for a variety of reasons, but one common one is that as you lose weight, your body needs fewer calories.
The next step: You could work on diet shifts or an increase in your exercise schedule to see if that gets things moving again. But you should also consider the possibility that you are at the weight that feels healthiest for your body. It’s helpful to talk about your personal ideal weight range with your provider. They can guide you on habit changes, dose adjustments, or considering another medication if needed.
If you’re stopping because you’re planning to conceive:
If you’re preparing for pregnancy, semaglutide needs to be stopped ahead of time. The medication stays in your body for 6 weeks on average, so giving yourself enough space before trying to conceive is important.
The next step: You should stop semaglutide 2 months before trying to get pregnant. This gives your body time to clear the medication.
Learn more: Semaglutide side effects in women: How they differ and how to manage them
If you’re stopping because you’re switching to another medication:
Some people stop semaglutide not because it’s a bad fit, but because another medication might work better for them, offer different coverage, or feel easier to manage. Switching is common and can be smooth with the right plan.
The next step: Your provider can help you time the switch so there’s no long gap between medications. This usually includes choosing the right starting dose, following the new titration schedule, and checking in after a few weeks to make sure the new option feels comfortable.
Learn more about how semaglutide compares to other medications:
Are you ready to stop taking semaglutide? Here’s what to ask yourself
Before stepping away from semaglutide, take some time to pause and check in with yourself. Think of this as a quick, gentle self-check to see if you feel prepared for the change and to help guide your next conversation with your provider.
You may not be ready to stop if:
- Your basic habits (eating, movement, sleep) still feel hard to keep up.
- You’ve seen quick regain after previous weight-loss attempts.
- You use semaglutide to help with conditions like diabetes, and haven’t talked through how stopping might affect them.
- You don’t have a clear plan for tapering or maintaining progress.
If any of this sounds familiar, slowing down the timing can make things smoother. Your provider can guide you toward a safer and more comfortable transition.
How to taper off semaglutide safely
If you and your provider decide it’s time to stop semaglutide, tapering can help you transition.
Here’s what a smooth taper can look like:
- Talk to your provider. They’ll look at your dose and how long you’ve been taking semaglutide, then help you choose a plan. A personalized taper helps prevent sudden appetite changes or blood sugar swings.
- They’ll lower the dose in small steps. You’ll move down little by little instead of stopping all at once. Slow changes give your body room to adjust.
- Give yourself enough time. A full taper can take a few weeks to a few months. A gradual pace helps your hunger cues, digestion, and energy stay steadier.
- Pay attention to small changes. You might notice hunger coming back sooner, shifts in mood or energy, or different blood sugar patterns if you have diabetes. Sharing these changes early helps your provider decide if the taper needs to slow down.
- Keep your daily habits steady. Balanced meals, movement you enjoy, and predictable sleep make this phase gentler on your body. These habits help hold the progress you’ve made, and tools like Noom can give extra structure if you want support during the transition.
Note: Medication changes must be supervised by a qualified healthcare professional.
When you need a maintenance dose or other medications
Stopping semaglutide doesn’t always mean stopping completely. Some people move to a smaller maintenance dose to help maintain a steadier appetite and weight.
But if semaglutide is no longer the best choice for you, there are other medications that might work better. Some are GLP-1s with different formulations, and others support weight in different ways. Your provider will help you compare choices and find something that fits your needs and comfort level.
Considering other GLP-1 medications
Semaglutide isn’t the only GLP-1 option that can support you. Other GLP-1 medications work in similar ways but may feel different in your body.
| Medication | Brand names and uses | Cost per month (without insurance) | Effectiveness | How it’s taken |
|---|---|---|---|---|
| Tirzepatide – GLP-1/GIP receptor agonist | Mounjaro®: type 2 diabetes, off-label weight loss Learn more Zepbound®: weight loss and obstructive sleep apnea (OSA) Learn more | Mounjaro®: $1,080Learn more Zepbound®: Pens: $1,086 Vials: $299 (2.5 mg), $399 (5 mg), $449 (7.5 mg, 10 mg, 12.5 mg, and 15 mg doses) Learn more | People lost an average of 21% of body weight at 72 weeks. | Weekly injection |
| Liraglutide – GLP-1 receptor agonist | Victoza®: type 2 diabetes, heart disease, off-label weight loss Learn more Saxenda®: weight loss Learn more Generic liraglutide: weight loss, type 2 diabetes, heart disease | Victoza®: $800 to $1,400 Learn more Saxenda®: $1,350 Learn more Generic liraglutide: $470 – $700 | People lost an average of 5-6% of body weight in one year. | Daily injection |
| Dulaglutide – GLP-1 receptor agonist | Trulicity®: type 2 diabetes, off-label weight loss Learn more | $987Learn more | People lost an average of 3-5% of body weight in 36 weeks. | Weekly injection |
Other medications
If GLP-1s aren’t the right match, there are other medication types you can try. Your provider may bring these up if they think a different kind of support would suit you better.
| Medication | Brand names | Cost per month (without insurance) | Effectiveness | How it’s taken |
|---|---|---|---|---|
| Metformin (off-label weight loss) | Glucophage®, Fortamet®, Glumetza® Learn more | Generic: $4–$20 Brand name: $100–$500+ Learn more | People lost an average of about 6% of their body weight over six months while taking metformin. | Pill taken up to two times daily |
| Phentermine | Lomaira®, Adipex-P® Learn more | $27-$100 Learn more | About 80% of people with a BMI of 30 or more lost at least 5% of their body weight in 6 months. | Daily pill |
| Diethylpropion | Tenuate®, Tenuate Dospan® Learn more | $40-$85 | People lost an average of 10% of their body weight in 6 months. | Pill taken one to three times daily |
| Naltrexone and bupropion | Contrave® Learn more | $600-$800 CurAccess™: $99 | People lost an average of 5 to 10% of their body weight in a year. | Pill taken up to twice daily |
| Orlistat | Xenical®, Alli® Learn more | $50-$800 | People in a study lost about 10% of their body weight after taking Orlistat for 1 year. | Pill taken three times daily with meals. |
| Phentermine and topiramate ER | Qsymia® Learn more | $180–$260 | People lost an average of 10% of their body weight in 56 weeks. | Daily capsule |
How to keep the weight off after semaglutide: Lifestyle changes
Once you stop semaglutide, the habits you practice every day make the biggest difference. Simple routines, such as how you eat, move, and rest, help you maintain weight loss.
Eat in a way that keeps you satisfied
Your meals and snacks matter even more once semaglutide isn’t helping lower your appetite. Choosing foods that fill you up and keep you steady can make your whole day feel easier.
Try steps like:
- Adding a lean protein source to every meal, like eggs, yogurt, chicken, tofu, or beans.
- Filling half your plate with fruits or veggies for fiber and fullness.
- Choose high-fiber carbs that help you feel satisfied.
Learn more: The complete guide to a high-protein diet for weight loss
Stay active in ways that feel doable
Movement helps keep your metabolism steady and protects your muscles. You don’t need complicated routines, just things you enjoy and can stick with.
You can start by:
- Walking, swimming, dancing, or doing any light activity for 10 to 15 minutes and building up to 150 minutes per week.
- Adding strength exercises (bodyweight squats, light weights, resistance bands) a couple of times a week.
- Using everyday movement—cleaning, running errands, taking the stairs—to stay naturally active.
Learn more: 4-week weight loss workout plan that you can do anywhere
Get better sleep and manage stress
How you sleep and manage stress can make a big difference in how steady your appetite feels after semaglutide. Small routines can help your body feel calmer and less “up and down.”
Try small changes like:
- Aiming for 7 to 9 hours of sleep.
- Using stress relievers, like breathing exercises or taking a short walk.
Get support
Maintaining a steady weight is simpler when you feel supported. One well-timed check-in or tracking habits can help you notice patterns and make changes. Noom can give you gentle structure, reminders, and a place to track the habits that keep you feeling steady.
Frequently asked questions about stopping semaglutide
You might still have a few questions as you think about stopping semaglutide, and that’s completely normal. This part is here to make things feel clearer and easier, so you know what to expect and what choices you have moving forward.
Do I need GLP-1 medications forever?
GLP-1 medications are made for long-term use, but that doesn’t mean you have to stay on them forever. Many people take semaglutide medications for 6 to 12 months, with some remaining on them for longer. The right choice for you depends on your body, routine, and goals.
Learn more: Understanding how long you can stay on Ozempic®
Is there a withdrawal syndrome?
Stopping semaglutide doesn’t cause a “withdrawal” syndrome, but you may feel changes as the medication fades out, such as a stronger appetite or a change in digestion.
Learn more: What happens when you stop taking Ozempic® or Wegovy®?
What’s the best time to restart if weight comes back?
There’s no one “right” moment. Some people restart when they see steady regain, others wait until they’ve tried adjusting their habits first. Your provider can help you figure out the safest timing based on your goals and how your body is responding.
Learn more: Is it safe to stop and restart Ozempic®?
Can you stop semaglutide cold turkey?
It’s possible, but not recommended. Stopping all at once can make appetite return quickly and may lead to blood sugar swings if you have diabetes. Tapering slowly helps your body adjust.
The bottom line: Have a plan in place when stopping semaglutide
Stopping a semaglutide medication can be a big change, but it doesn’t have to derail your progress. Once the medication effects fade, appetite usually returns, and digestion moves at its normal pace. That’s why some weight regain is common, but it’s not inevitable. What you do during the transition makes a big difference.
A gradual taper, steady routines, and habits that keep you full and energized—like eating enough protein, moving your body regularly, and getting consistent sleep—can help you stay on track. If you notice your hunger or weight changing more than expected, talking with your provider early can help you adjust your plan, whether that means restarting, switching medications, or fine-tuning your everyday habits.
The goal is staying aware of what your body needs as the medication leaves your system. With a clear plan and the right support, you can protect the progress you’ve made and move forward with confidence. Your provider can help you figure out the pace that feels right and talk through other treatment choices if you need them.
And for day-to-day support, Noom can help you create a plan that combines food tracking, exercise tips, and daily lessons to maintain weight loss for the long term.
Note: Ozempic®, Rybelsus®, Mounjaro®, Victoza®, metformin, and Trulicity® are not FDA-approved to treat obesity or for weight loss.
Editorial standards
At Noom, we’re committed to providing health information that’s grounded in reliable science and expert review. Our content is created with the support of qualified professionals and based on well-established research from trusted medical and scientific organizations. Learn more about the experts behind our content on our Health Expert Team page.